What is Laparoscopic Appendix Removal Surgery (Laparoscopic appendectomy)?
What is the appendix?
The appendix is a tube-like organ which is a few centimeters long. It is attached to the beginning of your large intestine, or colon. This is usually below and to the right of your belly button.
You probably know that the appendix can become inflamed. If the appendix needs to be removed, you can live without your appendix and not develop any long term issues.
What is appendectomy?
This is a type of surgery to remove the appendix. Removal of the appendix cures appendicitis. If appendicitis is untreated, it may rupture or burst open and cause very serious illness or even death.
Appendectomy is a common surgery and many people have had their appendix removed. One way to remove the appendix is by making one larger cut, or incision, below and to the right of your belly button. This is referred to as an open appendectomy.
Laparoscopic appendectomy removes the appendix using small incisions and will be described below.
How is a Laparoscopic Appendectomy Performed?
You will have general anesthesia for your laparoscopic appendectomy. This means that you are asleep during surgery. When surgery is finished, the surgeon closes your incisions with tiny stitches, staples, surgical tape or glue.
Once you are asleep, the surgeon makes an incision near your belly button and inserts a small device called a port. The port creates an opening that your surgeon can use to fill the abdomen with gas. This creates space to do the operation. Next, a small camera is inserted through the port. The camera shows the surgery on a screen in the operating room. Once the surgeon can see clearly, they put in more ports to insert long, narrow instruments.
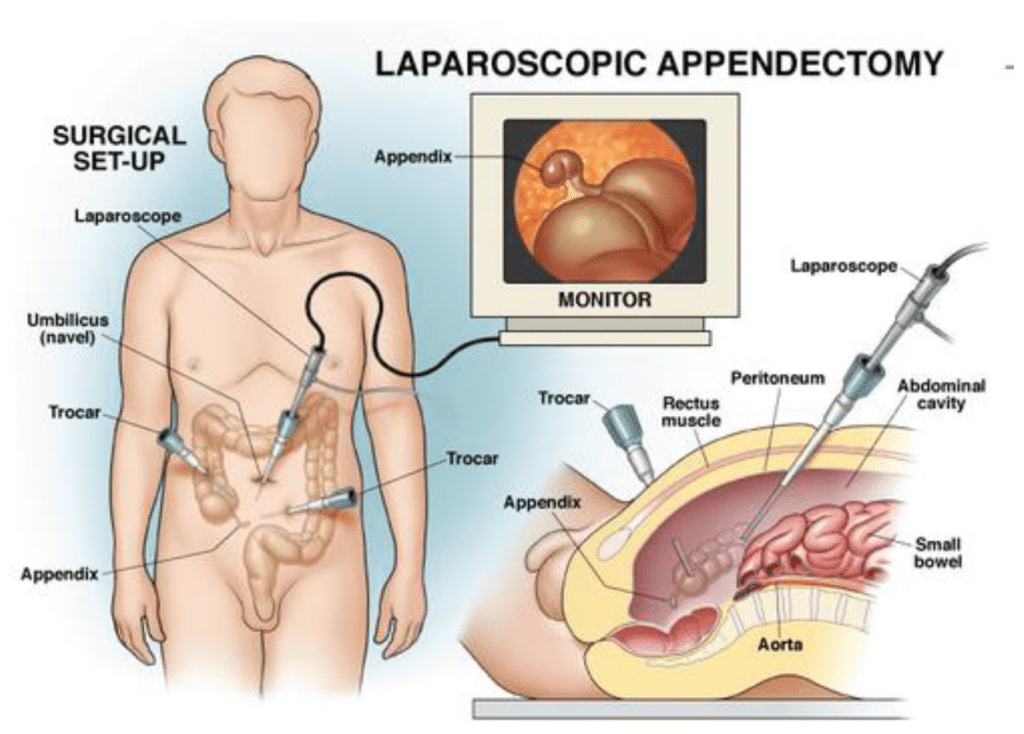
Finally, they gently disconnect your appendix and take it out through one of the incisions. Most operations need 3 incisions, but this can vary from 1 (one) to 4, based on various circumstances.
Your surgeon might use a surgical robot to do your operation. It is done the same way as described above. Your doctor guides the robot instead of guiding the instruments by hand. This is commonly referred to as robotic surgery.
Your surgery team might put in a small plastic tube called a “drain” during surgery. This lets fluid drain from the surgery area while you are healing, so it does not build up and cause problems. Your doctor will take out the drain later.
If the inflammation of your appendix is more complicated, a larger incision may be necessary to complete the surgery safely. Your surgeon will make this decision during the operation.
Advantages of laparoscopic appendectomy
The results may vary depending upon the type of surgery and your general health. But the most common advantages of laparoscopic surgery are:
- Less pain after surgery
- A shorter time in the hospital
- Getting back to normal activity faster
- Having normal bowel movements sooner
- A smaller scar
Is laparoscopic appendectomy right for you?
Ask your surgeon if a laparoscopic appendectomy is the best option for you. In certain situations, you might need surgery with one (1) larger incision.
What Happens if I cannot have my Appendix removed Laparoscopically?
Some people cannot have laparoscopic appendix removal. You might have open surgery with one large incision if you are one of these people. Some reasons for having or switching to open surgery are:
- Your appendix is very inflamed or there is an abscess (a large area of bacteria buildup).
- Your appendix has perforated (burst).
- You have severe obesity – this means being extremely
- You have scar tissue in your abdomen from earlier surgery or
- The doctor cannot see your organs
- You have bleeding problems during
It is not a complication (problem) if your surgeon decides to switch to open surgery. They will switch if open surgery is the safest option for you. Your surgeon might not know this until after the laparoscopy starts. They will use their best judgment about the safest surgery for you.
What are the Possible Complications of Laparoscopic Appendectomy?
Complications of laparoscopic appendectomy do not happen often. They can include bleeding, infection in the surgery area, hernias, blood clots, and heart problems. A hernia is a hole that allows a small amount of your gut (intestine) or other tissue to bulge through the muscles that cover it.
You should also know that any surgery has the risk of hurting other body parts. This is not likely, but it is possible. Appendix surgery could hurt nearby areas such as the bladder, large intestine (colon), or small intestine. You might need another surgery if this happens.
There is a small risk of an abscess (collection of pus/bacteria) following surgery if the inflammation of the appendix is severe at the time of surgery. This may require further treatment.
Most complications from appendectomy are rare, which means they almost never happen. If you are concerned about any possible complications, ask your surgeon.
What to Expect After Surgery
What Should I Expect after Appendectomy? Going home
You may go home the day you have your surgery, or you might stay in the hospital overnight. You need to be able to drink liquids before you go home. If the appendix had already perforated (burst), you may be in the hospital for a longer period of time.
Will I be in pain?
You will feel some pain after surgery. Pain at the incision sites and in your abdomen is common. You might also have pain in your shoulders. This is from the carbon dioxide put into your abdomen during the operation. The shoulder pain should go away in 24 to 48 hours.
You can take non-prescription medications to relieve pain, unless your doctor tells you not to take over-the-counter medications. Acetaminophen (Tylenol®) and ibuprofen (Advil®) are examples of non-prescription pain medications. Putting ice on your incisions can also help. Ask your doctor or nurse about the correct way to use ice.
Your surgeon might prescribe a small amount of narcotic pain medicine to help you with pain. Many people recover from surgery without taking any narcotic pain medicine, but some will need narcotics for a few days. If you have questions about pain after surgery, ask the surgeon or your nurses. They should be able to tell you how long the pain will last and what to expect.
You might feel sick to your stomach (nauseated) or throw up (vomit) after your surgery. Having surgery and anesthesia can make this happen. You should feel better in a day or two. Tell your doctor or nurse if you keep vomiting or feeling nauseated.
Activities
You should be as active as your body allows. Doctors recommend walking. You can go up and down stairs on the day of your surgery. The next day, you may take your bandages off, if you have them, and take a shower. You can expect to feel a little better each day after going home. If not, please call your doctor.
You can probably go back to normal activity about a week after laparoscopic appendectomy.
If you do a physical job with heavy lifting, ask your doctor when you can go back to work. You can drive 24 hours after you have had anesthesia if you are not taking narcotic pain medicines and not in pain.
If you had an open surgery with a large incision, you may need more time to recover. Your surgeon will advise you when you may return to normal activities. You will probably recover more slowly in other ways, too. Your doctor can tell you what to expect.
When to see your doctor after surgery
You need to see your surgeon 1 to 4 weeks after surgery.
When to Call Your Doctor After Laparoscopic Appendectomy
Be sure to call your surgeon or family doctor if you have any of the problems below.
- Fever over 101 degrees F (38.5 C)
- Severe pain or swelling in the belly
- Feeling sick to your stomach or throwing up (nausea or vomiting) – Call your doctor if you cannot eat or
- Blood or pus coming from any of the small cuts in the surgery area – Or redness that spreads or gets
- Pain that your medicines do not help
- Breathing problems or a cough that does not get
Call your doctor’s office if you have any other questions about your recovery.
This brochure is not intended to take the place of talking with your doctor about appendectomy. If you have any questions about your need for an appendectomy, other tests, billing and insurance coverage, or your doctor’s training and experience, please ask your doctor or their office staff. If you have questions about appendectomy or your care after this procedure, please ask your doctor before or after the examination.
Brought to you by:
SOCIETY OF AMERICAN GASTROINTESTINAL AND ENDOSCOPIC SURGEONS (SAGES)11300 West Olympic Blvd., Suite 600
Los Angeles, CA 90064
- Tel:
- (310) 437-0544
- E-Mail:
- publications@sages.org
- Revised:
- April 1, 2020
