Balazs I Lengyel, MD, Ali Tavakkolizadeh, MD. Department of General Surgery, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA, USA; Surgical Planning Laboratory, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA, USA
INTRODUCTION: The purpose of this study is to determine whether 3D model based volumetric analysis can predict surgical outcome more reliably than a one-axis splenic length measurement in order to provide a better pre-procedural evaluation for Laparoscopic Splenectomy (LS). Laparoscopy has become the standard approach for elective removal of the spleen for both benign and malignant indications. Pre-operative assessment generally includes a CT scan to measure splenic size, using maximal splenic length as a surrogate marker of anticipated surgical difficulty. This method is commonly used, with some using a length above 20 or 25cm as a contraindication to a laparoscopic approach.
METHODS AND PROCEDURES: We analyzed 72 patients who had undergone LS between 1997 and 2006 in our institution. Outcomes including estimated blood loss (EBL), operative room times (OR time), and length of stay (LOS), were collected and correlated to maximal recorded splenic length. We then gathered contrast enhanced CT images for 15 patients, and created 3D reconstruction with manual segmentation of the spleen and calculated the splenic volume using 1-mm slices and the free source 3D Slicer software [Figure 1]. Linear regression was used to analyze splenic length and splenic volume as a predictor for EBL, OR time, and LOS. Time to complete the modeling for each patient was recorded.
RESULTS: There was no association between splenic length and EBL, OR time, or LOS, highlighting that this pre-operative measurement is a poor predictor of surgical difficulty in LS. Splenic volume was however a significant predictor of OR time (p=0.017, R2=0.52). Reconstruction of spleen models including segmentation, data loading and model rendering took an average of only 13.2 minutes for each patient [Figure 2].
CONCLUSION: Volumetric analysis can be a valuable tool for predicting surgical difficulty in LS. With the use of available free source software, pre-operative 3D assessment can support surgical planning, with minimal additional time. Further studies looking at splenic volume versus outcomes will result in better selection of patients suitable for laparoscopic approach.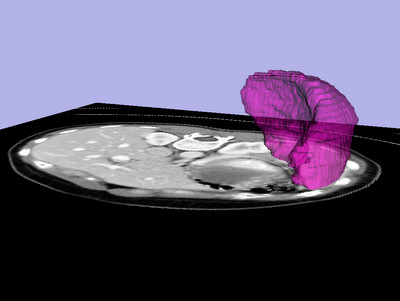
Figure 1. 3D reconstructed model of the spleen
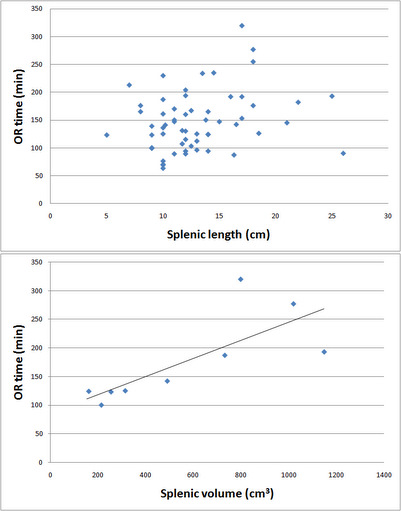
Figure 2. Splenic volume as a predictor of OR time
Session: SS17
Program Number: S098