Bindhu Oommen, MD, MPH, Samuel W Ross, MD, MPH, Joel F Bradley, MD, Kristopher B Williams, MD, Hannah C Kline, Vedra A Augenstein, Brant T Heniford, MD, Ronald F Sing, DO. Carolinas Medical Center, Department of Surgery, Division of Gastrointestinal & Minimally Invasive Surgery, Charlotte, NC.
INTRODUCTION Percutaneous endoscopic gastrostomy (PEG) tube placement is a valid mechanism of enteral support when oral feeding is contraindicated or not possible and is commonly performed by both surgeons and gastroenterologists. Our objective was to compare outcomes of PEG placement by surgeons versus gastroenterologists (GI).
METHODS AND PROCEDURES: A retrospective chart review of patients undergoing PEG tube placement at our institution between May 2011 and May 2013 was performed. Demographics, comorbidities, perioperative details, complications, hospital length of stay (LOS), and mortality were collected. Univariate analysis was performed with p <0.05 deemed statistically significant.
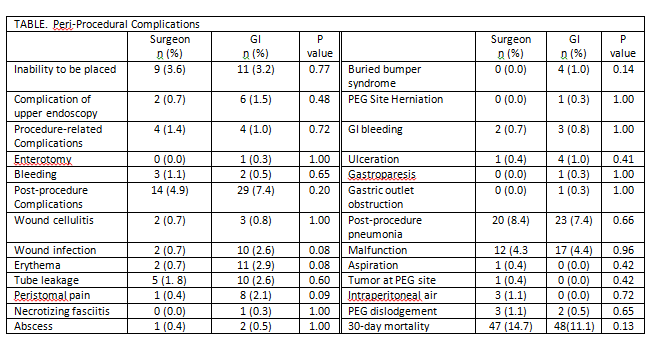
RESULTS: Over the two-year period, 643 patients had PEG tubes placed: 273 (42.5%) by surgeons, 370 (57.5%) by GI. Comparing surgeons vs. GI, a higher number of PEG tubes were placed on an inpatient basis by surgeons (92% vs 73%; p<0.001). In both groups, 62% were male; 68% Caucasian. Surgeons operated on slightly younger patients (56.0 ±19.8 vs 64.3 ±13.5 years; p<0.001). Comparing surgeons to gastroenterologists, GI tended to place PEGs in more comorbid patients: CAD (8.1% vs 13.0%), history of cancer (12.1% vs 35.1%), hypertension (38.8% vs 53.2%), anti-platelet therapy (25.8% vs 36.1%), risk of aspiration (20.0% vs 36.1%), pneumonia (31.6% vs 19.1%); all p<0.05. Illicit drug use (5.3% vs 1.4%) and respiratory failure as indicated by tracheostomy at any time during admission (58.7% vs 16.8%) were higher in the surgeon group; p<0.05. When PEG placement was by a surgeon, concomitant tracheostomies were performed in 48% of cases, compared to 14% in GI group (p<0.001). The most common indications for PEG were CNS impairment (43% vs. 35%), dysphagia (34% vs. 31%), enteral access (12% vs. 4%), oropharyngeal neoplasm (6% vs. 25%), and gastric decompression (5% vs 6%); p<0.001. Although overall intraoperative and postoperative complications were higher among GI, they were not statistically significant (p>0.05). The pre-procedure LOS (13.8 vs 9.1 days; p<0.0001) and post-procedure LOS (13.0 vs 5.1 days; p<0.0001) were longer in the surgeon group.
CONCLUSIONS: Surgeons and gasteroenterologist have similar technical outcomes and no significant difference in complications. The longer LOS in the surgeon group may be attributed to prolonged respiratory failure.