Kevin L Chow, MD, Hassan Mashbari, MD, Mohannad Hemdi, MD, Eduardo Smith-Singares, MD. University of Illinois at Chicago
Introduction: Esophageal trauma represents an uncommon but potentially catastrophic injury with a reported overall mortality of up to 20%. The management of iatrogenic and spontaneous perforations have been previously described with well-established guidelines which have been mirrored in the trauma setting. Esophageal leaks are the most feared complication after primary surgical management and present a challenge to salvage. There has been increasing reports in the literature supporting the use of removable covered metal stents to treat esophageal perforations and leaks in the non-trauma setting. We present the first reported case series of four patients presenting with external penetrating trauma induced esophageal injuries, complicated by failure of initial primary surgical repair and leak development, successfully managed with the use of esophageal stents.
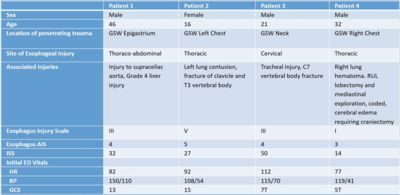
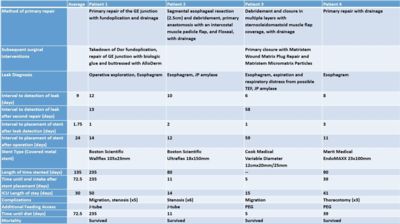
Materials and methods: A retrospective review was performed at a Level I trauma center identifying four patients who underwent endoscopically placed removable covered metal stents, either by a surgical endoscopist or an interventional gastroenterologist, after failure of primary surgical repair of esophageal traumatic injuries. Demographic information, hospital stay, additional interventions, complications, imaging studies, ISS scores, and outcomes were collected.
Results: Our cohort consisted of 4 patients with penetrating injuries to the chest and neck with esophageal injuries (3 thoracic and 1 cervical esophageal injuries) managed with esophageal stenting after leaks were diagnosed following primary surgical repair. Their initial esophageal injuries included grades 1, 3 and 5. Leaks were diagnosed on average post-operative day 9. Two patients underwent an additional attempted surgical repair and subsequent leak development. Esophageal stents were placed under endoscopic and fluoroscopic guidance within 3 days of leak diagnosis. There was resolution of their esophageal fistulas with all patients resuming oral intake (averaging 72 days after stent placement). Three patients (75%) required further endoscopic interventions to adjust the stent due to migration or for dilations due to strictures. Mortality was 0%, all patients survived to be discharged from the hospital with average ICU length of stay of 30 days.
Conclusion: The use of esophageal stenting has progressed over the last few years, with successful management of both post-operative upper gastrointestinal leaks as well as benign, spontaneous, or iatrogenic esophageal perforations. While the mainstay of external penetrating traumatic esophageal injuries remains surgical exploration, debridement, and repair with perivisceral drainage; our case series illustrates that the use of esophageal stents is an attractive adjunct that can be effective in the management of post-operative leaks in the trauma patient.

Presented at the SAGES 2017 Annual Meeting in Houston, TX.
Abstract ID: 86840
Program Number: P374
Presentation Session: iPoster Session (Non CME)
Presentation Type: Poster