Carter C Lebares, MD, Stanley J Rogers, MD. UCSF
BACKGROUND: Duodenal fistulas are uncommon but morbid complications of acute necrotizing pancreatitis. If percutaneous drainage fails, surgical correction via roux-en-Y diversion or pancreaticoduodenectomy can be required. While self-expanding metal stents have been tried, complications like migration and perforation have limited such use. Endoscopic transmural stents have successfully treated fistulas of the stomach, particularly post-sleeve gastrectomy. Here we present a case of endoscopic transmural stents used to treat a non-resolving duodenal fistula following acute necrotizing pancreatitis.
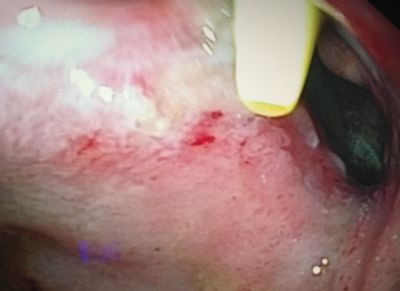
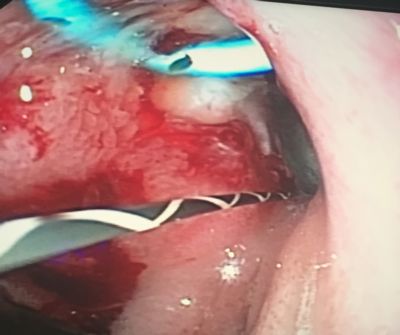
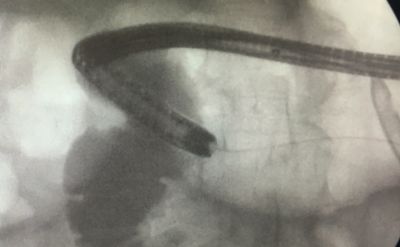
METHODS: Under general anesthesia, using a standard adult gastroscope, the fistula was identified in the second portion of the duodenum (Fig 1). A flexible-tipped guide wire was used to identify the fistula tract and two 7Fr 5cm double pigtail biliary stents were deployed (Fig 2) with positioning verified under fluoroscopy. Two weeks later these were removed and a single stent deployed into the visibly smaller tract (Fig. 3). Two weeks after that, the single stent was removed and contrast medium was injected under fluoroscopic visualization, demonstrating resolution of the fistula (Fig 4).
CASE: This patient is a 72 year old woman with hypertension and congenital hearing loss who underwent a cholecystectomy for biliary colic and subsequent ERCP with sphincterotomy for retained stone. This was complicated by acute pancreatitis which progressed to severe necrotizing pancreatitis with infected retroperitoneal necrosis. Percutaneous drainage yielded initial improvement but a persistent moderate collection (300cc per day) lead to the identification of a fistula in the second part of the duodenum. Repositioning and exchange of percutaneous drains over 8 weeks did not hasten resolution. Endoscopic transmural pigtail stents were tried after visualization of a large (8-10mm diameter) fistula tract. Stents were utilized as described in Methods, with a total of three endoscopic interventions, at 2 week intervals, resulting in resolution of the fistula as evidenced by contrast injection into the duodenum under fluoroscopy and subsequent CT scan with oral contrast. The patient’s symptoms resolved and she was tolerating a normal diet. She remained thus at 1 month follow-up.
CONCLUSION: This case demonstrates the benefit of endoscopic transmural stents for the resolution of duodenal fistulas, expanding the utility of this technique to address leaks and fistulas of the upper gastrointestinal tract. Further study is warranted to clarify the timing and adjuncts to optimize the use of this promising approach.

Presented at the SAGES 2017 Annual Meeting in Houston, TX.
Abstract ID: 88574
Program Number: P131
Presentation Session: iPoster Session (Non CME)
Presentation Type: Poster