Hassan Mashbari, MD, Kevin L Chow, MD, Mohannad Hemdi, MD, Kirstie K Danielson, PhD, Eduardo Smith-Singares, MD. University of Illinois at Chicago
Introduction: Complex pancreatic and duodenal injuries due to trauma continue to present a formidable challenge to the trauma surgeon with a described mortality of 5-30% and morbidity of 22-27%. Duodenal fistula formation subsequent to failure of attempted primary repair is associated with significant morbidity and mortality. We present the first reported series of four patients with complex trauma-related duodenal injuries who had failure of primary repair which were managed with duodenal stenting. We compared outcomes to a matched case control cohort of patients with trauma related duodenal injuries. The aim of this study is to document our experience with enteral stents in patients with complex duodenopancreatic traumatic injuries.
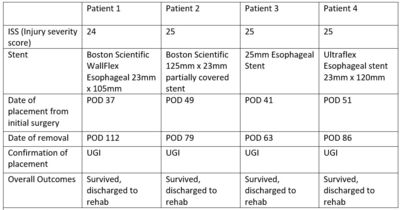
Methods: A retrospective review at a Level I trauma center identified 4 patients who underwent endoscopically placed indwelling covered metal stents after failure of primary duodenal repair in the form of high output duodenal fistulas. A matched case control cohort was identified including 6 patients with duodenal fistulas who were not treated with stents. Drainage volumes were collected and classified according to source and phase of intervention (i.e. admission to fistula diagnosis, to stent insertion, after removal, and until discharge).
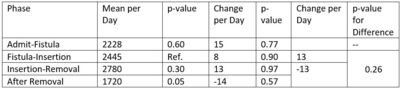
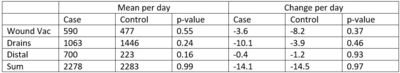
Results: There was a decrease in the mean combined drain output of 497ml/day (p=0.16) after stent placement. When comparing the sum of all output sources, there was a statistically significant difference across phases (p=0.03) and “After Removal” was significantly less when compared to the reference phase (p=0.05). There was also a change in the directionality of the slope for the sum of all drain outputs with an increase of 13 ml/day2 prior to stent placement compared to a decrease of 13ml/day2 (p=0.26) after stent placement. The stenting group demonstrated a decrease in mean drain output (1063ml/day vs 1446ml/day, p=0.24) and increase in distal gastrointestinal output (700ml/day vs 223ml/day, p=0.16). One patient in the stent group required later operative repair. All other patients in the stenting and control group had resolution of their fistulas over time. There were 2 late mortalities in the control group.
Conclusion: The stent treated patients demonstrated diversion of approximately 500ml/day of enteral contents distally. While all patients eventually healed their fistulas, the stent treated patients demonstrated an accelerated abatement of drain outputs when compared to the control cohort, but did not reach statistical significance. Indwelling enteral-coated stents appear to be an effective rescue method for an otherwise inaccessible duodenal fistula after failure of primary repair.
Presented at the SAGES 2017 Annual Meeting in Houston, TX.
Abstract ID: 87858
Program Number: P373
Presentation Session: iPoster Session (Non CME)
Presentation Type: Poster