Stefania Marconi, MSc1, Andrea Pietrabissa, PhD, MD2, Ferdinando Auricchio, PhD3. 1Dept. of Surgical Sciences, Dept. of Civil Engineering and Architecture, University of Pavia, 2Dept. of Surgical Sciences, University of Pavia, 3Dept. of Civil Engineering and Architecture, University of Pavia
Objectives
The aim of the work is the use of 3D printing technology to build patient-specific models for procedure planning in laparoscopic surgery, especially for splenectomies and live donor kidney procurements. Our goal is improving the way surgical procedure are planned, thanks to the informative power of physic objects with respect to conventional imaging systems. The final goal is the integration of these facilities in the daily clinical practice, considering their importance also for educational purposes and as a support for the explanation of the surgical procedure to patients.
Materials and Methods
We start form Multi Detector Computed Tomography (MDCT) image elaboration to virtually reconstruct the patient-specific anatomy: MDCT images are acquired using a contrast dye with a slice-thickness resolution of at least 2 mm. For spleen models only arterial contrastographic phase is used, while for renal models also the late phase is used to reconstruct ureters.
Through the use of an open source software, ITK-Snap (https://www.itksnap.org), we apply a segmentation algorithm that identifies and marks with a specific label the structure of interest in each MDCT slice. Therefore, arteries, veins, ureters and the various parenchymal structures are identified with different labels. The resulting label set can be rendered to get a 3D virtual model of each anatomical structure. Each model is then exported using the STL (Standard Tessellation Language) file format that can be processed for the 3D printing: the STL model is sliced into layers of the same thickness of 3D printer resolution. For our purpose, we use an Objet 30 Pro 3D printer, able to deploy layers up to 16 microns of thickness. The high-resolution is mandatory to reproduce all the fine details of anatomical structures, especially the vascular ones. Models are printed with a white rigid photo-polymeric material, which is deployed in a liquid form and cured with UV light during the printing process.
The image elaboration procedure takes from 1 to 3 hours, depending on image quality, while the printing of each model takes up to 23 hours: after the printing, each structure is painted in different colours and assembled.
Results
Up to now we produced 16 patient-specific 3D printed models: 12 for laparoscopic splenectomy and 4 for live donor kidney procurement. Among splenectomy models, 10 were investigated to assess their ability in transferring detailed information, especially to young surgeons. Moreover, the usefulness of the 3D printed models for the patient comprehension of the surgical procedure has been qualitatively assessed.
Conclusions
3D printed models of patient-specific anatomy can give an important aid to surgical planning, since they can transfer information in a more immediate way: the possibility of hold in hand the model can significantly improve the quality of the planning. Models usefulness is quite evident for young surgeons, since they have less experience in building a mental 3D reconstruction of the specific anatomy. Through this facility, both novice surgeons and patients have the possibility of better understanding the surgical procedure.
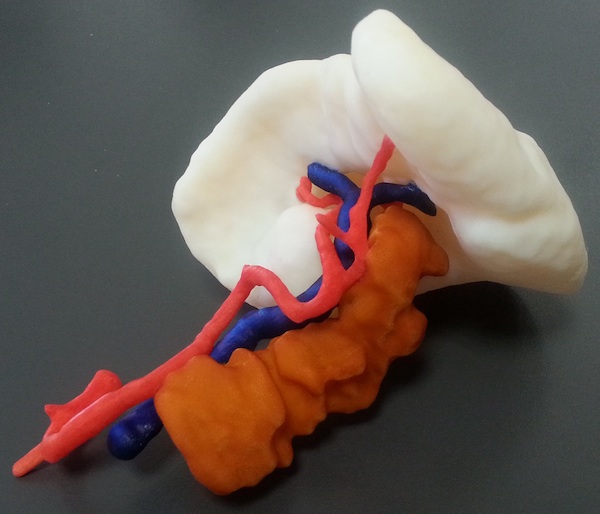
Fig. 1: Example of a 3D printed model for laparoscopic splenectomy.