This may be a difficult subject matter for you and your patient to talk about. Be assured, all major organized religious groups encourage and recommend the COVID-19 vaccine. Listed below are references and websites you can direct your patient towards to help them make an informed decision with regards to their religious concerns against the COVID-19 vaccine.
Pope Francis video message approving the COVID-19 Vaccine
https://www.catholicnewsagency.com/news/248714/pope-francis-ad-council-collaborate-to-promote-covid-19-vaccines-in-the-americas
Statement from the Vatican approving the COVID-19 Vaccine
https://press.vatican.va/content/salastampa/en/bollettino/pubblico/2020/12/21/201221c.ht
Catholic US Bishops approve the use of the COVID 19 Vaccine
https://www.catholicnewsagency.com/news/46899/catholic-us-bishops-approve-use-of-covid-19-vaccines-with-remote-connection-to-abortion
Christian Connection for International Health Vaccine Campaign
https://www.ccih.org/wp-content/uploads/2020/03/Faith-Leaders-COVID-Vaccine-Factsheet.pdf
Central Conference of American Rabbis Support COVID-19 Vaccinations
https://www.ccarnet.org/ccar-responsa/nyp-no-5759-10/
Orthodox Union COVID-19 Vaccination Guidance
https://rabbis.org/wp-content/uploads/2020/12/Guidance-re-Vaccines.pdf
Dalai Lama Urges other to get vaccinated
https://www.bbc.com/news/world-asia-india-56310274
National Muslim Task Force and the National Black Muslim COVID Coalition (NBMCC) on Ramadan 2021 and COVID-19 Vaccines
https://isna.net/wp-content/uploads/2020/04/Press-Release-NMTF-Ramadan-Statement-4.6.2021.pdf
Church of Jesus Christ of Latter-Day Saint approve vaccination
https://www.churchofjesuschrist.org/church/news/church-makes-immunizations-an-official-initiative-provides-social-mobilization?lang=eng&query=vaccination
Jehovah’s Witness “Are Jehovah’s Witnesses Opposed to Vaccination? NO”
https://www.jw.org/en/jehovahs-witnesses/faq/jw-vaccines-immunization/
List compiled 9-30-2021





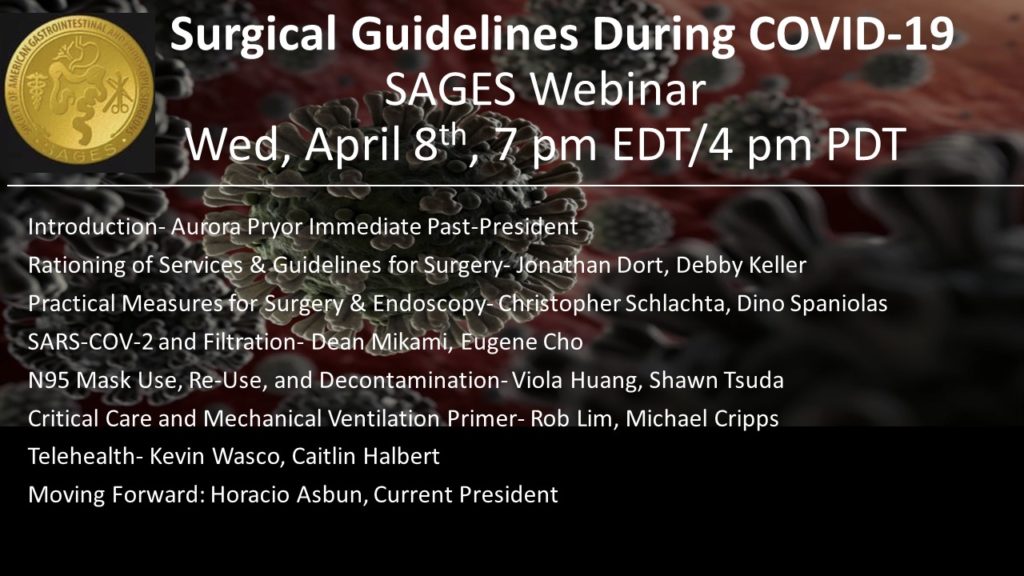

 These are uncertain times for all of us facing the COVID-19 pandemic. As surgeons, we are seeing a halt to our elective practice, a transition to virtual clinic visits, and potential redeployment into areas of the front line in ICUs or medical wards that are outside of our regular practice patterns. Healthcare workers overall are facing potential equipment shortages, including in personal protective equipment. SAGES is working hard to provide resources to help you navigate this unfamiliar landscape. I can’t believe it was only two weeks ago that we postponed our annual meeting until August.
These are uncertain times for all of us facing the COVID-19 pandemic. As surgeons, we are seeing a halt to our elective practice, a transition to virtual clinic visits, and potential redeployment into areas of the front line in ICUs or medical wards that are outside of our regular practice patterns. Healthcare workers overall are facing potential equipment shortages, including in personal protective equipment. SAGES is working hard to provide resources to help you navigate this unfamiliar landscape. I can’t believe it was only two weeks ago that we postponed our annual meeting until August.