Krista Hardy, MSc MD, Josephine Kwong, BScH MPA, Kristen Pitzul, BScH MSc, Ashley Vergis, MD MMed, Timothy Jackson, MD MPH, David Urbach, MD MSc, Allan Okrainec, MD MHPE. University of Manitoba, Winnipeg, Man., Department of General Surgery, University Health Network, University of Toronto, Toronto, Ont., Canada
Introduction: The benefits of laparoscopic surgery in the management of colon cancer have been well established. Controversy remains in the application of this technique in rectal cancer. The objective of this study was to compare the early outcomes and total hospital cost of laparoscopic (lap) and open rectal surgery.Methods and Procedures: Patients undergoing elective lap or open rectal resection at the University Health Network, University of Toronto from April 2004 – March 2009 were included. Patient demographic, operative (OR) and outcome data was obtained from electronic hospital records. Cost data was determined from the hospital case costing system and median costs were compared using the Mann-Whitney U Test. Conversions to open surgery were analyzed on an intention-to-treat basis. Binary logistic regression analysis was used to compare differences in baseline patient characteristics. Pathology reports were reviewed for tumor status, nodal harvest and resection margins. The relationship between length of stay and cost was determined with analysis of covariance.
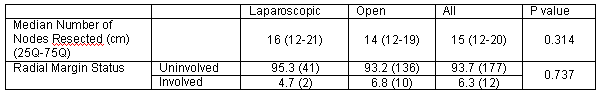
Results: There were 68 (26%) lap and 191 (74%) open rectal resections. The rate of conversion to open surgery was 28.8%. There was no difference in preoperative body mass index, gender, American Society of Anesthesiology score or Charlson Index. Open patients were more likely to have a previous laparotomy (40.8 vs 17.6 %, open vs lap, p= 0.001). Most patients had a final pathologic diagnosis of invasive cancer (85.1 vs 81.7, lap vs open, p=0.525). Median operative time was slightly longer for lap surgery (291 vs 254 min, lap vs open, p=0.005), while median length of stay was less for lap surgery (6 vs 8 days, lap vs open, p=0.000). Rates of neoadjuvant therapy were similar for invasive cancers. There was no difference in T status, N status, number of nodes resected or margin status (Table). Complication rates were similar (21.2% vs 22.0%, lap vs open, p=1.000). There were no differences in ICU admissions, reoperations, 30-day readmissions or emergency room visits. Lap surgery was associated with higher operative cost ($4 656.56 vs $4 292.79, lap vs open, p=0.014) but lower ward cost ($4 050.96 vs $5 222.61, lap vs open, p=0.003). Total hospital cost was similar for lap and open surgery ($11 661.79 vs $12 449.34, lap vs open, p=0.097) Length of stay was a significant predictor of cost (p=0.001).
Conclusion: The laparoscopic approach was associated with similar short term outcomes and shorter length of stay. Examination of costs revealed a similar total hospital cost for both procedures with higher operative and lower ward costs associated with laparoscopic approach. This study is consistent with previous literature supporting the short term benefits of laparoscopy and furthermore demonstrates comparable costs between procedures.
Session Number: Poster – Poster Presentations
Program Number: P104
View Poster