Jed F Calata, MD, Gopi Tripuraneni, MD, Jasna Coralic, MD, Kunal Kochar, MD, John J Park, MD, Slawomir Marecik, MD, Leela M Prasad, MD
Advocate Lutheran General Hospital, Division of Colon and Rectal Surgery
Introduction
Ureterocolic fistulas secondary to diverticular disease are rare, and usually occur in patients following a long protracted history. We describe a case in a patient who had experienced sporadic symptoms over six months. To our knowledge, there are only seven other published cases of ureterocolic fistulae secondary to diverticular disease.
Case Description
An 80 year old woman presented with a four day history of left iliac fossa (LIF) and left flank pain associated with nausea and vomiting. The patient also complained of urinary frequency without dysuria, and a rusty discoloration of her urine. Significant past medical history included an episode of diverticulitis six months prior. On physical examination the patient was febrile with a temperature of 380C, tachycardic with a pulse rate of 120 bpm, and blood pressure of 120/70 mm Hg. There was no abdominal tenderness, and PV and PR examinations were unremarkable.
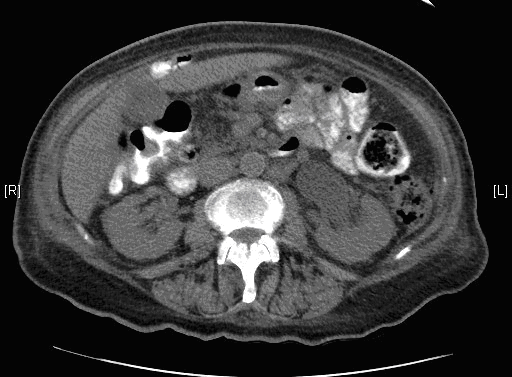
An abdomino-pelvic computer tomography scan with intravenous contrast revealed a sigmoid mass with evidence of intramural gas consistent with a pelvic abscess extending to the left pelvic side wall, with partial left ureteric obstruction and moderate hydronephrosis (Figure1).
Cystoscopy, Ureteroscopy and retrograde Pyelography revealed a fistula communicating with the sigmoid colon (Figure 2). A double J ureteric stent was inserted to cover the fistula and relieve the ureteric obstruction. On flexible sigmoidoscopy, there was only evidence of diverticulosis, and the fistula was not visualized.
She underwent a hand assisted laparoscopy which confirmed a large abscess at the pelvic brim involving the left lateral pelvic wall. The left ureter was encased in the abscess cavity which upon drainage, revealed the ureterocolic fistula. The diseased segment of the sigmoid colon was excised, and a colostomy fashioned in the left lower quadrant.
Discussion
The incidence of diverticulosis is 33-66%. Fistulae secondary to diverticulitis occur in approximately 1%. Ureterocolic fistulae are uncommon. Ureterocolic fistulae usually occur secondary to tuberculosis, Crohn’s disease, and pelvic malignancies. Fistulae secondary to diverticulitis in contrast are rare.
Of the seven previously reported cases of ureterocolic fistula secondary to diverticular disease, the age of incidence (range 45-88) coincides with the overall peak incidence of diverticular disease in population. All of the patients, except one, had a history of urological symptoms and left iliac fossa pain. All of the patients had a protracted illness, ranging from four weeks to ten years.
Barium enemas were the most useful diagnostic investigation in these patients, and were positive for ureterocolic fistula in four of five patients. In our case, cystoscopy, ureteroscopy and retrograde pyelogram, thought to be of little diagnostic value, helped define and confirm the fistula preoperatively.
Spontaneous closure of fistulae is rare, and requires resection of the diseased colonic segment. Also, if the function of the underlying involved kidney is poor, a nephroureterectomy may be performed.
Conclusion
Ureterocolic fistulae secondary to diverticular disease are rare.
However, it is important to be aware of the diagnoses due increasing incidence of diverticular disease in an aging population.
Session: Poster Presentation
Program Number: P674