Samuel W Ross, MD, MPH, Blair A Wormer, MD, Bindhu Oommen, MD, MPH, Mimi Kim, MD, John D Watkins, Amanda L Walters, MS, Vedra A Augenstein, MD, Brant T Heniford, MD. Carolinas Medical Center, Dept. of Surgery, Division of Gastrointestinal and Minimally Invasive Surgery.
INTRODUCTION: Large PEHR can be challenging to plan pre-operatively given the multiple options for surgical repair. We hypothesized that greater dimensions of paraesophageal hernia (PEH) on pre-operative CT of would predict the need for salvage techniques in PEHR.
METHODS AND PROCEDURES: We queried our prospectively collected, institutional hernia-specific database for all PEHR from 2008 to March 2013. Only PEHR with pre-operative CT of the chest and/or abdomen were included. CT measurements of defect and hernia sac were obtained using transverse, coronal and sagittal views. Area and volume were calculated using standard formulas. CT measurements, esophageal length on upper endoscopy, and recurrent hernia status were then analyzed by operative techniques and patient outcomes using standard statistical methods; significance set at p≤0.05.
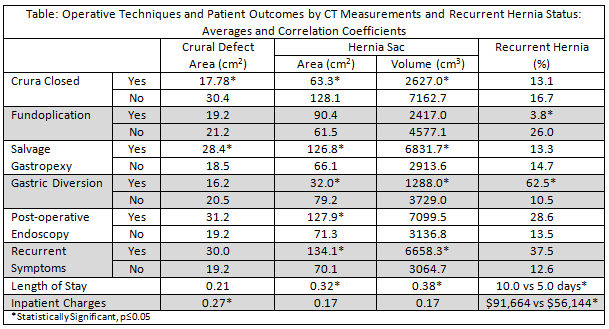
RESULTS: There were 103 laparoscopic PEHR, with three conversions to open. Mean age was 63.8±11.7 years, BMI was 30.2±12.8 kg/m2, and esophageal length was 35.2±3.7cm. The population was 35.0% male, 12.6% diabetic, 8.7% smoker. Distribution of PEH by classification was 17.5% Type I, 1.9% Type II, 57.3% type III and 23.3% Type IV PEH; 13.6% were emergent and 14.6% recurrent. There were no Collis gastroplasties; biologic mesh was used in 65.1%, and fundoplication was performed in 51.5%. Average CT measurements were as follows: defect width 4.5±2.0cm, depth 6.8±3.0cm, area 19.4±15.7 cm2; sac length 7.8±3.5cm, width 10.3±5.0cm, depth 6.8±3.1cm, area 74.4±59.1 cm2, volume 3,369±3,723 cm3. The crura could not be closed in 17.7%: salvage gastropexy was performed in 13.6%, and gastric diversion in 7.8%. Average length of stay was 5.8±6.9 days and inpatient charges were $61,285±48,749. There was a 4.6% recurrence rate, 6.3% required post-operative endoscopy, 7.3% had recurrent symptoms and there was one death. Operative techniques and patient outcomes association with pre-operative CT measurements are presented in the Table. Mesh use, reoperation, readmission, incisional hernia formation, and death were not associated with increased CT measurements or recurrent hernia; p>0.05. Esophageal length did not correlate with any operative techniques or outcomes; p>0.05.
CONCLUSION: Repair of large PEH requires a variety of techniques to adequately prevent reherniation and recurrent symptoms. Pre-operative CT measurements of defect area, hernia sac area and volume correlate with increased use of operative salvage techniques, post-operative complications, and charges. CT can be a valuable adjunct in operative planning and risk assessment in large and recurrent hernias. Additionally, recurrent hernia is an indicator that gastric diversion or other salvage technique is required.