Cristina A Metildi, MD, Sharmeela Kaushal, PhD, Santiago Horgan, MD, Mark A Talamini, MD, Robert M Hoffman, PhD, Michael Bouvet, MD. University of California San Diego Department of Surgery; AntiCancer, Inc., San Diego
Introduction: The aim of this study was to evaluate the autofluorescent properties of bile and the subsequent utility of fluorescence cholangiography to facilitate intraoperative identification of biliary anatomy in mice.
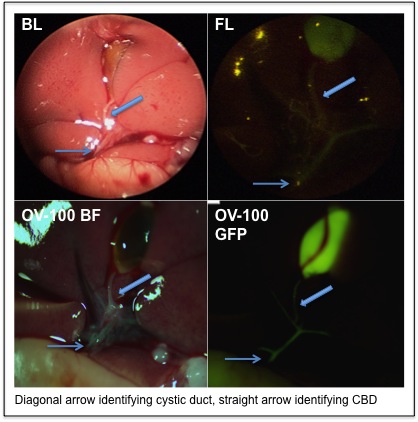
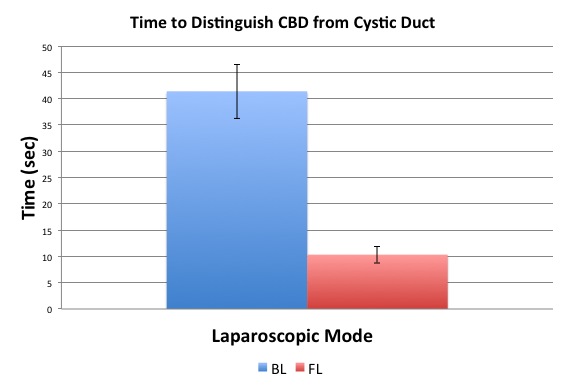
Methods: Diagnostic laparoscopy was performed on four to six week old athymic mice under bright and fluorescence light. Standard bright light laparoscopy (BL) was achieved with a Stryker X8000 xenon light source. Fluorescence laparoscopy (FL) was achieved by placing a 495-nm emission filter between the Stryker L9000 LED light source and a Stryker 1288 HD camera. To achieve mouse laparoscopy, a 2.7 mm 0° laparoscope was inserted through a 3 mm trocar mid-abdomen and secured with a purse string suture. Insufflation was set to a pressure of 2 mm Hg, which permitted sufficient pneumoperitoneum for adequate visualization and manipulation of the laparoscope within the abdominal cavity. Post laparoscopy, the mice were sacrificed and their abdomens exposed for intravital imaging with the OV-100 Small Animal Imaging System to serve as a visualization control. The parameters measured were time to distinguish the common bile duct (CBD) from the cystic duct and the subject’s ability to correctly identify additional biliary anatomy.
Results: Utilizing the autofluorescence of bile in the mouse model improved the subjects’ ability to identify the cystic duct, decreasing the mean time from 37.3 seconds under bright light to 7.6 seconds under fluorescence light (p<0.001). More importantly, time to distinguish the cystic duct from the CBD was also significantly decreased with fluorescence cholangiography (41.4s under bright light vs. 10.3s under fluorescence light, p<0.001). Additionally, fluorescence cholangiography afforded the subjects greater ease in further identifying multiple hepatic ducts. While only 36% of additional biliary anatomy was correctly identified under BL, fluorescence cholangiography permitted proper identification of 80% of biliary anatomy (p<0.001). Overall, fluorescence cholangiography was significantly associated with accurate identification and localization of complete biliary anatomy among all subjects (p=0.014).
Conclusions: The autofluorescence of bile facilitated real-time identification of biliary anatomy in mice during laparoscopy. Fluorescence cholangiography could improve real-time intraoperative identification of biliary anatomy during laparoscopic procedures without additional need for an intraoperative cholangiogram. This technique has potential to decrease the incidence of iatrogenic biliary tract injuries during laparoscopic cholecystectomy without significantly adding to operative time.
Session Number: Poster – Poster Presentations
Program Number: P393
View Poster